
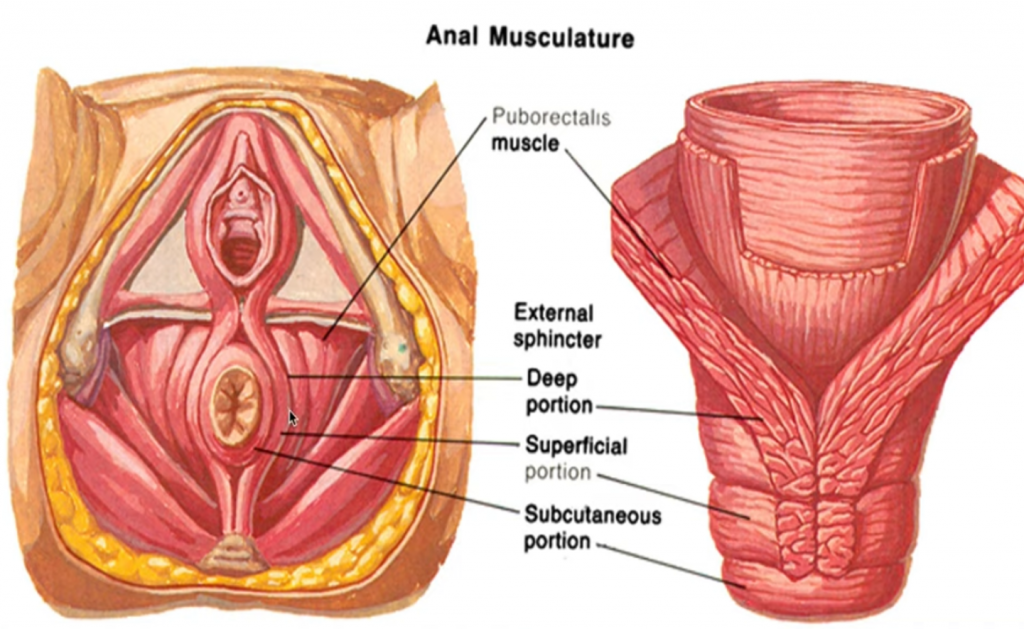
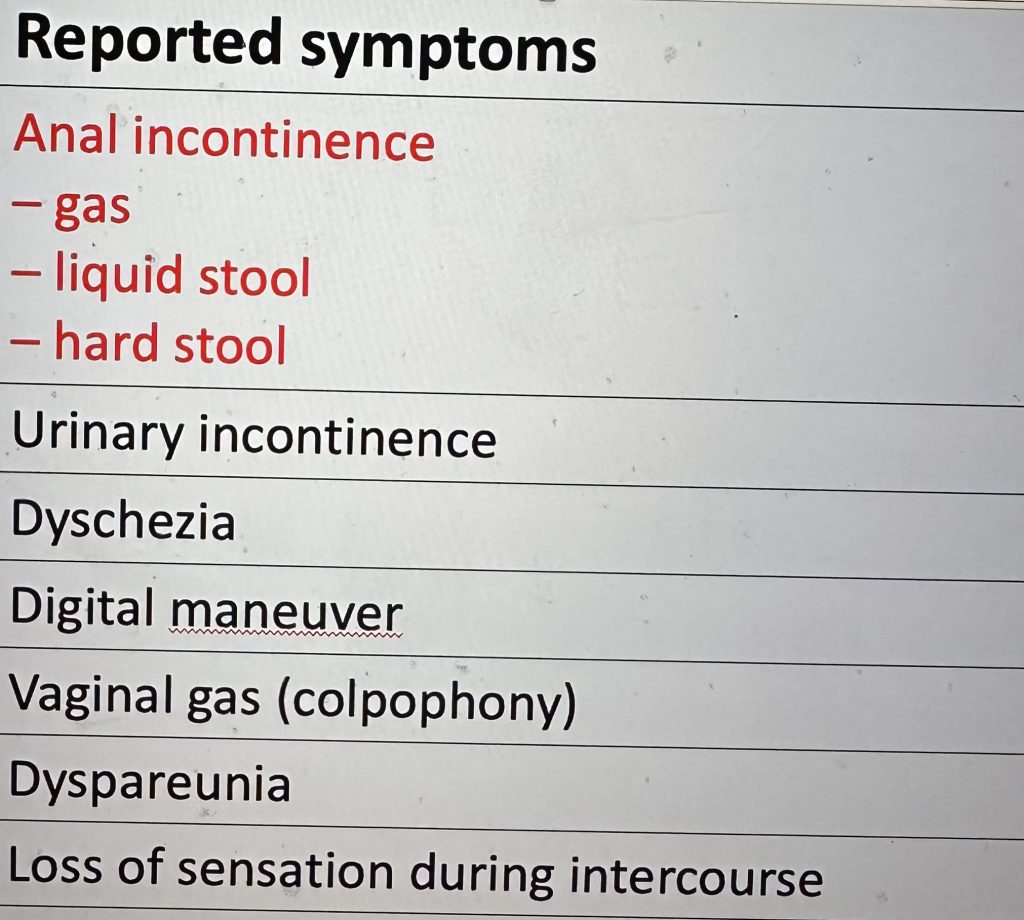
Anal sphincter incontinence (ASI): results from a functional impairment of ≥1 of the anatomic components that allow normal continence:
•the internal anal sphincter (IAS)
•the external anal sphincter (EAS)
•the pelvic floor muscles (puborectalis)
•the anal cushions that ensure adequate rectal compliance
•the sensory-motor apparatus
Mechanisms:
•Sphincter defects -perineal tearing, stretching and/or ischemia:
•Obstetrical trauma – OASIS (childbirth trauma, episiotomy)
•Proctologic surgery (keyhole deformity)
•degeneration of the pelvic floor muscles, which appears with aging and particularly after the menopause as the pelvic floor structures are hormone-sensitive
Sphincter repair surgery is proposed for large defects of either the EAS, IAS, or both:
•Acute (fresh) anal sphincter and perineal injury -direct reconstruction of the muscle injury by end-to-end sphincter suture.
-If there is no available surgical specialist, primary repair can be delayed 8–12 h without worse outcomes at 1-year follow-up
-Delayed primary repair is usually not recommended routinely
•Older defects – a secondary sphincter repair (overlaping) also gives good results as long as the LA muscle has a good function
-a delay of at least 6 months to 1 year has been recommended to allow the tissue to recover
Short-term outcomes with anterior sphincteroplasty of the EAS are excellent or good in terms of continence, with a 71% to 86% improvement